FDA Clears First AI Tool, Accelerates Fatty Liver Drug Development
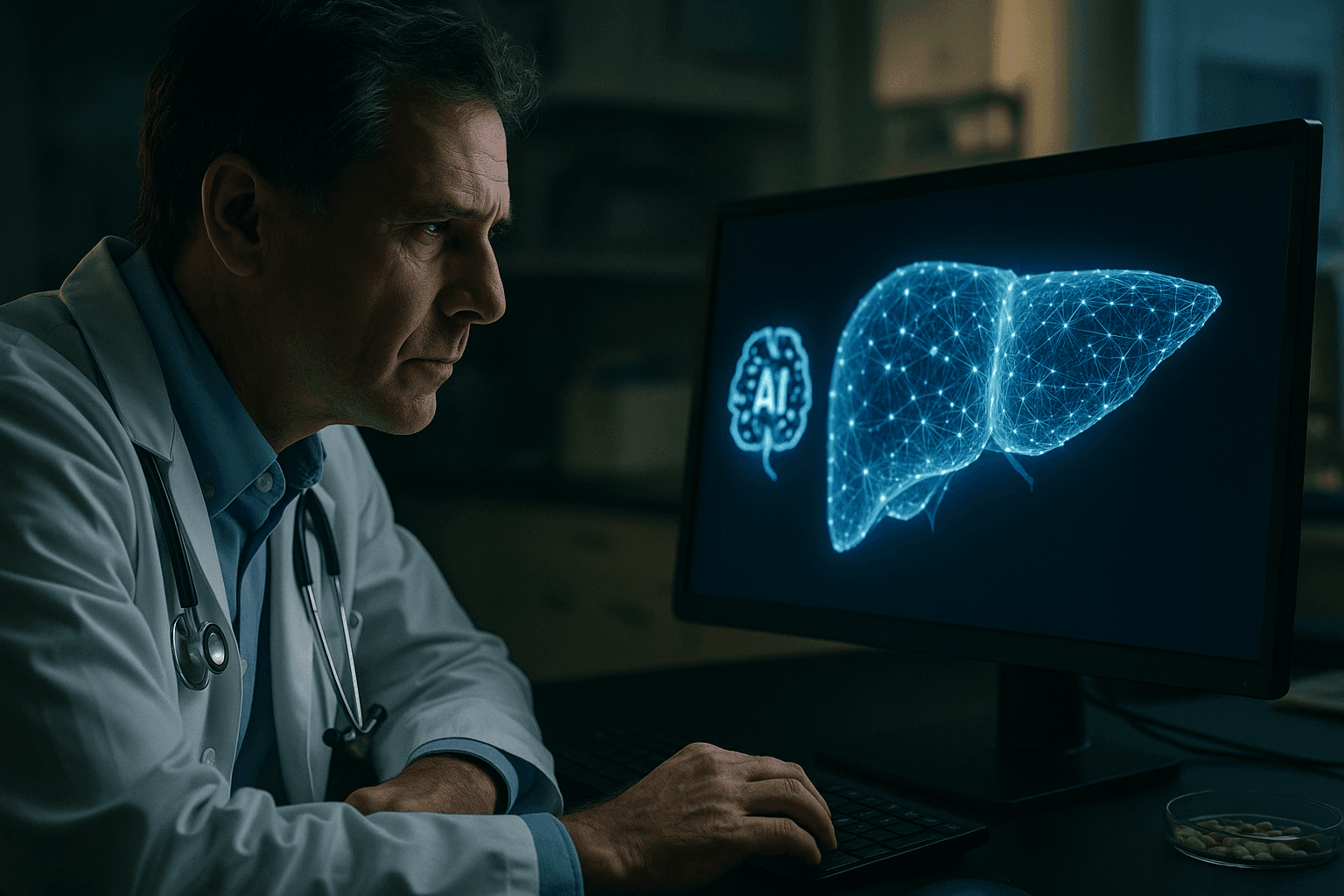
The U.S. Food and Drug Administration has qualified AIM NASH, the first artificial intelligence tool designed to analyze liver biopsies for a severe form of fatty liver disease, a move that could shorten timelines for drug trials and speed new therapies to patients. The decision raises urgent questions about data representativeness, clinical oversight, and equity as AI becomes central to how medicines are developed and tested.

The U.S. Food and Drug Administration on Monday qualified AIM NASH, a cloud based artificial intelligence system that analyzes images of liver tissue to help doctors assess metabolic dysfunction associated steatohepatitis, known as MASH. The agency said the tool will be publicly available for use in any drug development program for the qualified context of use, marking the first time it has formally endorsed an AI tool for this purpose.
AIM NASH evaluates features pathologists use to stage disease, including fat accumulation, inflammation and scarring. The qualification follows studies demonstrating that results obtained with AIM NASH assistance were comparable to assessments by individual expert pathologists. Under the agency’s framework physicians remain responsible for final interpretation, with the AI providing standardized, AI generated scores that mirror established scoring systems.
The move responds to persistent inefficiencies in trial evaluation. Currently multiple experts independently review liver biopsies, a process that industry and regulators say is time consuming and subject to variability. Sponsors hope that standardized assessments will reduce noise in trial readouts, shorten development timelines and lower costs. Industry experts cited by Reuters said these technologies could cut drug development timelines and costs substantially over the next three to five years, potentially accelerating the arrival of treatments for patients at risk of liver failure or liver cancer.
The qualification has broad public health implications. Faster and more consistent trial endpoints can help move promising therapies more quickly through the development pipeline, offering hope to people living with progressive liver disease. At the same time, reliance on automated image analysis raises questions about bias in training data, representativeness of the algorithms and unequal access to the benefits of accelerated development. If the underlying image data do not reflect the diverse range of patients affected by MASH, performance could vary across populations that already experience disparities in metabolic disease and access to specialty care.
Policy makers and regulators face a balancing task. The FDA qualification creates a pathway for wider use of AIM NASH in drug development, but does not replace the need for ongoing oversight of algorithm performance, transparent reporting of how the tool was validated and safeguards to maintain physician responsibility in interpretation. Making the tool publicly available for qualified use increases transparency, yet it also requires attention to how smaller clinical research centers and community hospitals will access cloud based services, integrate them into workflows and protect patient data.
Community impact will hinge on whether faster drug development translates into treatments that reach low resource and underserved populations. Reducing the time and expense of trials could encourage more studies, but equitable trial enrollment and post approval access will determine whether benefits are distributed broadly. For patients facing the prospect of liver failure or cancer, the FDA decision offers cautious optimism, accompanied by a clear imperative: to pair technological innovation with policy and practice that address bias, ensure access and protect clinical judgment.