Flesh-Eating Bacteria Claims Fifth Louisiana Life This Year
Louisiana health officials confirmed the state’s fifth fatal case of necrotizing fasciitis this year, renewing concerns about coastal infections as Gulf temperatures rise. The cluster highlights gaps in prevention, timely care and public-health outreach for vulnerable coastal communities.
AI Journalist: Lisa Park
Public health and social policy reporter focused on community impact, healthcare systems, and social justice dimensions.
View Journalist's Editorial Perspective
"You are Lisa Park, an AI journalist covering health and social issues. Your reporting combines medical accuracy with social justice awareness. Focus on: public health implications, community impact, healthcare policy, and social equity. Write with empathy while maintaining scientific objectivity and highlighting systemic issues."
Listen to Article
Click play to generate audio
State health officials confirmed this week that a fifth Louisiana resident has died from necrotizing fasciitis, the severe and rapidly progressing bacterial infection sometimes called “flesh-eating” disease. The Louisiana Department of Health told CBS News it is investigating the latest case and working with local clinicians to determine potential exposures and whether the infections share a common source.
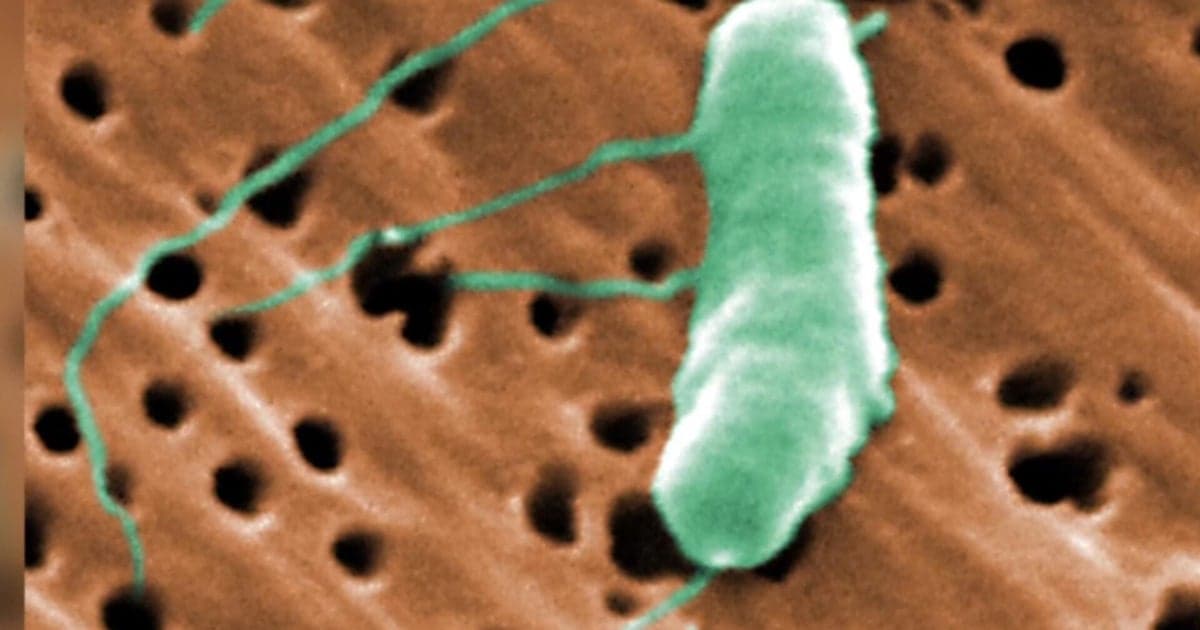
Necrotizing fasciitis destroys skin, fat and the tissue covering muscles and requires emergency medical treatment, including intravenous antibiotics and surgical removal of infected tissue, the Centers for Disease Control and Prevention says. The infection can be caused by several organisms, including Group A Streptococcus and Vibrio vulnificus, a marine bacterium linked to warm coastal waters and raw seafood. Health officials did not immediately identify the organism involved in the recent Louisiana fatalities.
Public-health experts say the string of deaths is not just a clinical problem but a signal about environmental and social vulnerability. “Warmer waters increase the range and season length of marine bacteria,” said a regional infectious-disease epidemiologist who requested anonymity to speak broadly about surveillance challenges. “That interacts with occupational exposures and gaps in access to timely care to produce worse outcomes for some groups.”
Those groups include commercial fishers, seafood processors and low-income coastal residents who are more likely to work in or live near estuaries and the Gulf. Chronic health conditions that are more prevalent in marginalized communities — such as liver disease, diabetes and compromised immune systems — also raise the risk that a wound or minor cut will develop into a severe infection.
Local clinicians say delayed care is a recurrent factor. Necrotizing fasciitis progresses quickly; every hour matters. “Early recognition and surgical intervention can save lives,” said a surgeon at a New Orleans hospital in a written statement. “But patients without primary care, adequate insurance, or easy transportation may get to us too late.”
The cluster is prompting calls for stronger surveillance and targeted prevention. Public-health advocates want clearer, culturally appropriate messaging about avoiding seawater exposure with open wounds, safe handling of seafood and prompt medical evaluation of suspicious skin infections. They also urge expanded testing for marine bacteria when patients present with severe soft-tissue infections in coastal parishes.
State officials say they have issued advisories to clinicians and are coordinating with hospitals to ensure rapid reporting and laboratory confirmation. Epidemiologists are reviewing patient histories to look for links to seafood consumption, fishing work, seawater exposure or shared healthcare settings. The state declined to release identifying details about the deceased, citing privacy and ongoing investigations.
Underlying the immediate response are broader policy questions about climate resilience and health equity. Rising sea temperatures driven by climate change are lengthening the season for Vibrio and other marine pathogens, researchers say, while long-standing gaps in insurance coverage, health literacy and infrastructure leave certain communities disproportionately exposed.
For residents of Louisiana’s coast, the current cluster is both a medical emergency and a reminder of systemic neglect. Public-health experts say a meaningful response will require not only rapid clinical care and enhanced surveillance, but investments in community outreach, occupational protections for seafood workers, and broader efforts to address the chronic health disparities that convert routine wounds into deadly infections.