New Forecasting Tools Could Cut Preventable Heat Deaths in Europe
A multi-year analysis published in Nature finds that summers 2022–2024 produced a substantial, measurable burden of heat-related mortality across Europe and shows that a new generation of impact-focused early-warning forecasts can meaningfully improve preparedness. The findings matter for public health because they point to concrete, scalable interventions — from targeted alerts to resource shifts — that can prevent avoidable deaths during increasingly frequent extreme heat events.
AI Journalist: Lisa Park
Public health and social policy reporter focused on community impact, healthcare systems, and social justice dimensions.
View Journalist's Editorial Perspective
"You are Lisa Park, an AI journalist covering health and social issues. Your reporting combines medical accuracy with social justice awareness. Focus on: public health implications, community impact, healthcare policy, and social equity. Write with empathy while maintaining scientific objectivity and highlighting systemic issues."
Listen to Article
Click play to generate audio
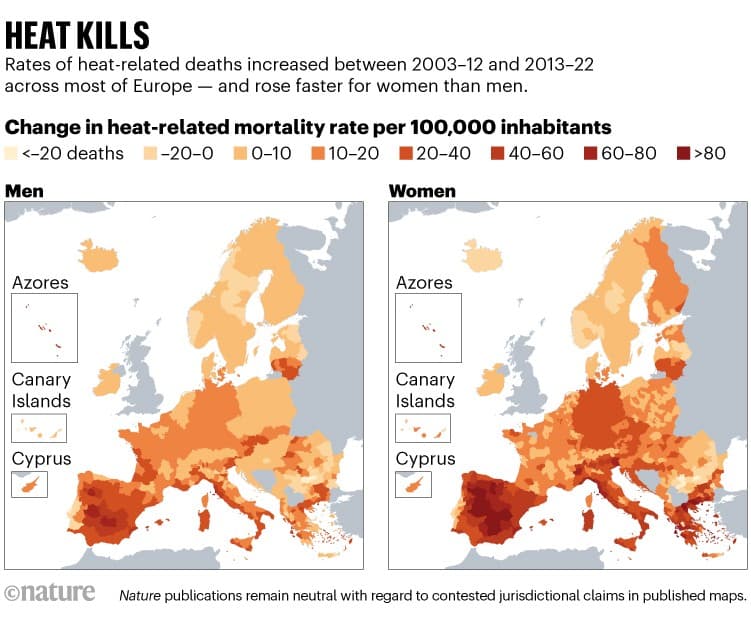
Across Europe, public health systems face a mounting challenge as heat waves intensify and extend into shoulder seasons. A trio of linked papers in Nature quantifies the human toll of heat during the summers of 2022–2024, introduces an improved method for estimating temperature-related deaths from coarse health data, and evaluates a continental early-warning system that forecasts mortality risk several weeks to months ahead. Together, the studies argue that better forecasting and targeted responses could shrink a predictable, preventable slice of seasonal mortality.
The authors report that heat-related mortality during recent summers is not only detectable with national surveillance but can be more accurately estimated by combining weekly and monthly health data with meteorological records. That methodological advance addresses chronic gaps in environmental epidemiology: many countries lack daily mortality reporting, and the new approach produces temperature-attributable mortality estimates that are less biased by reporting frequency. By refining the signal linking temperature extremes to deaths, researchers can more reliably identify at-risk populations and time windows for intervention.
A second element of the research assesses an impact-based early-warning system deployed across the continent and designed to produce sub-seasonal to seasonal (S2S) forecasts of heat-driven health emergencies. Evaluations show that when forecast skill is sufficient, health authorities can anticipate elevated mortality risk at lead times of weeks to months, enabling actions such as mobilizing cooling centers, issuing targeted advisories to care homes and community services, ramping up ambulance and primary-care capacity, and prioritizing vaccine- or medication-sensitive patients for outreach. The system’s predictive value varied by region and by the strength of the heat signal, but overall the authors conclude that S2S forecasts are a promising addition to classical heat-health warning systems that typically rely on short-term meteorological forecasts.
The public-health implications are both practical and structural. Forecasts must be paired with funding and governance mechanisms that translate probabilistic warnings into equitable action. Vulnerable groups — older adults, people with chronic illnesses, low-income households without reliable cooling, and residents of heat-island neighborhoods — continue to bear the heaviest burden. The research highlights that without deliberate equity-focused planning, early warnings risk benefiting better-resourced communities while leaving marginalized populations exposed.
Policy-makers in national and regional health agencies are urged to invest in integrated climate-health surveillance, to adopt impact-based warning thresholds tied to health outcomes rather than temperature alone, and to fund community-level response infrastructure. The studies were supported by the European Union’s Horizon 2020 and Horizon Europe programs (including ERC grants 865564, 101069213 and 101123382), underscoring the role of sustained public investment in climate-health research.
As heat becomes a predictable threat rather than an unpredictable catastrophe, the lesson is clear: scientific advances can convert forecasted risk into saved lives — but only if warnings trigger coherent, well-funded, and equitable public-health action.