Senate Rejects Competing Plans, ACA Subsidies Face Expiration
The Senate rejected two party line proposals on Dec. 11 and Dec. 12, leaving enhanced Affordable Care Act premium tax credits poised to expire at year end and putting millions of Americans at risk of higher insurance costs. Lawmakers offered dueling approaches, but the failure to reach a compromise shifts the fight to the House and leaves families and insurers scrambling for certainty.
In back to back procedural votes this week the Senate declined to advance two competing measures that sought to address COVID era enhancements to Affordable Care Act premium tax credits, effectively leaving those subsidies on track to lapse at the end of the year. The two party line proposals failed on Dec. 11 and Dec. 12, a result widely characterized as a political exercise in a deeply divided Congress rather than an earnest effort at bipartisan compromise.
Democrats put forward a bill to extend the enhanced premium tax credits for three years, arguing the continuation is essential to keep marketplace coverage affordable for millions of enrollees. Republicans countered with a framework led by Sens. Mike Crapo of Idaho and Bill Cassidy of Louisiana that would have expanded or created new health savings accounts and provided one time payments to help consumers with out of pocket costs, a plan aimed at reshaping choices within private coverage rather than temporarily extending subsidies.
Both proposals failed to draw cross party support. Coverage characterized the votes as largely symbolic, and Alabama Sen. Katie Britt warned, "Real Americans are paying the price for this body not working together in the way it should." Senate Majority Leader John Thune placed the competing measures on the floor, and Republican leaders pushed the GOP framework despite uncertainty among some senators about whether it would win backing. Senators Lisa Murkowski of Alaska, Susan Collins of Maine and Rick Scott of Florida had not signaled firm votes for the GOP plan, underscoring intraparty divisions.
Critics of the Democratic extension said it would be an expensive short term fix and that more comprehensive changes to the ACA are needed. Opponents of the Republican approach argued that expanded health savings accounts and one time payments would be inadequate to cover the premiums and medical costs faced by most consumers. Those competing critiques, relayed by health policy reporters, help explain why neither measure attracted bipartisan support.
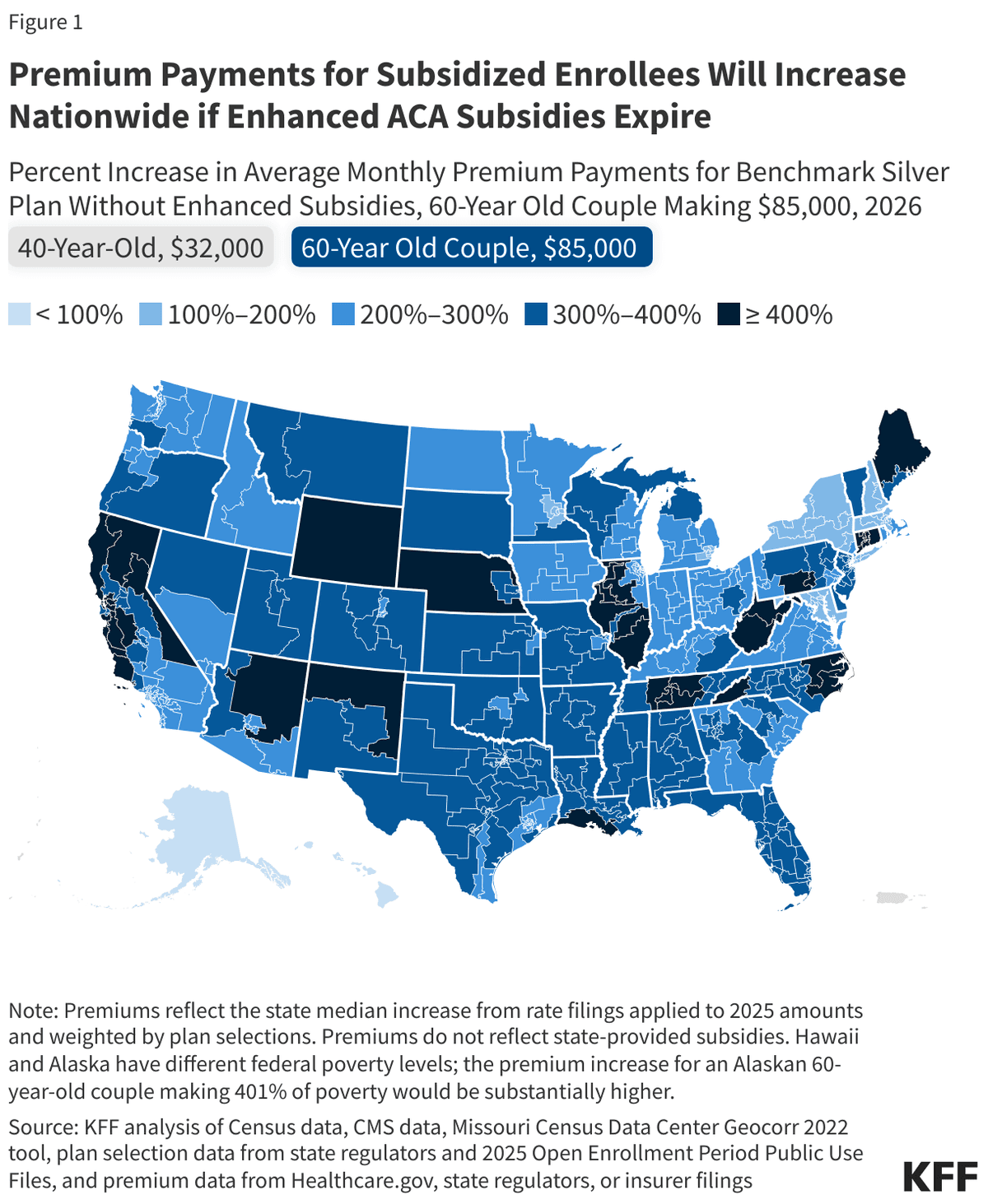
The practical consequence of inaction is stark. Enhanced premium tax credits have been credited with substantially lowering monthly premiums and increasing enrollment since they were expanded during the pandemic. With their likely expiration, millions of people who receive marketplace subsidies could face steep premium increases in January, and analysts warn that overall health care costs for many households will spike. Insurers and state markets face uncertainty as open enrollment and renewal notices move forward without clarity about federal support.
The battle now shifts to the House, where Speaker Mike Johnson has promised a vote "next week" amid visible Republican fractures. Some House Republicans, particularly moderates in competitive districts, are pressing for short term relief, while conservatives seek broader changes. Rep. Kevin Kiley has been identified as pushing for a short extension, but it remains unclear whether the House can pass a measure that would survive political and procedural hurdles.
With deadlines looming and millions of people reliant on subsidies, lawmakers face a choice between a brief extension to preserve current coverage affordability or a broader rewrite that could reshape private insurance markets. The consequences for families and state budgets will be immediate if Congress fails to act.
Know something we missed? Have a correction or additional information?
Submit a Tip
