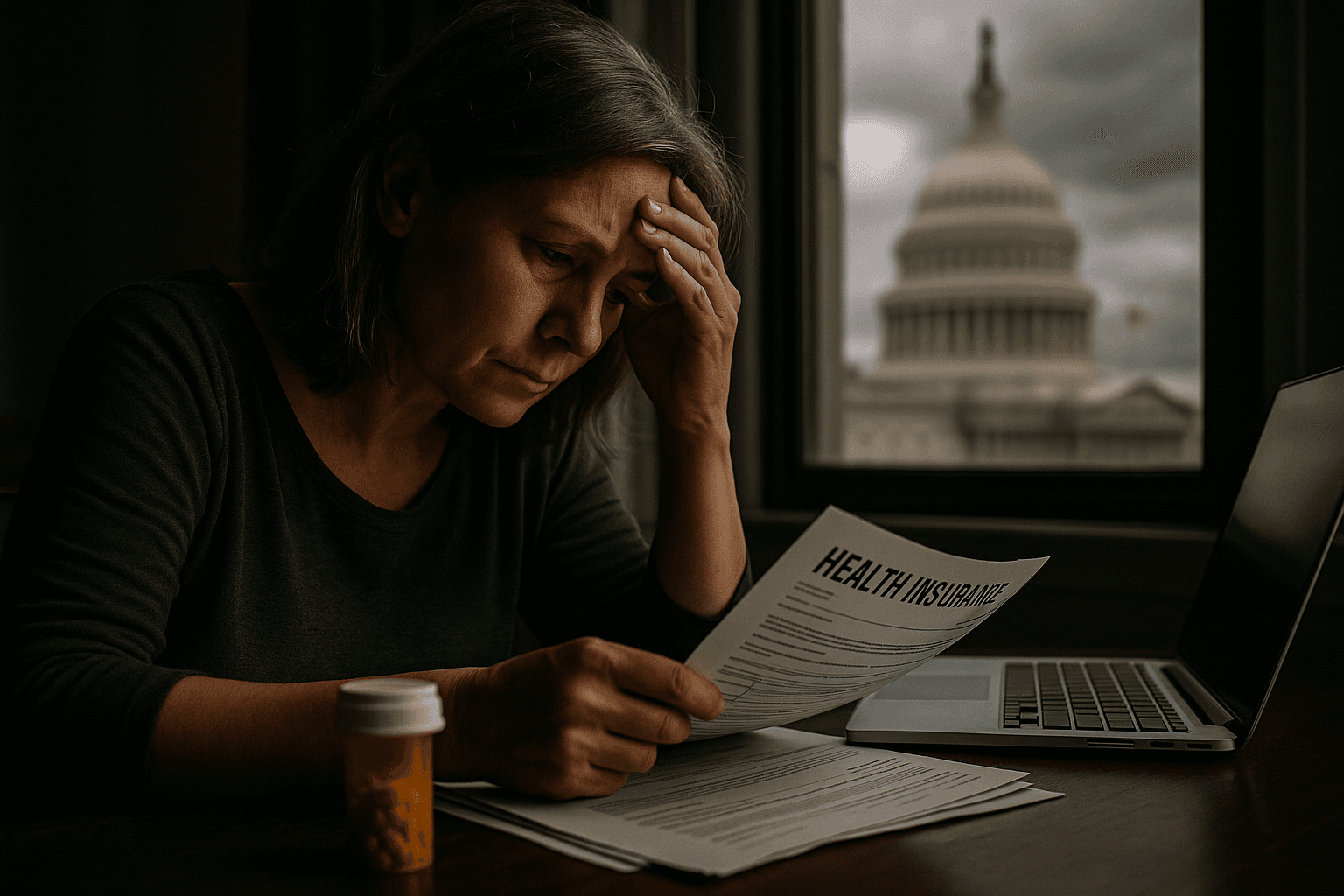
Senate Set to Reject ACA Subsidy Extension, Millions Face Higher Costs
The Senate appears poised to vote down legislation that would keep Affordable Care Act tax credits in place, a move that could drive steep premium increases for millions who buy insurance on the marketplaces starting January first. The failure to reach a bipartisan agreement underscores deep political divisions and raises urgent questions about access to care, financial strain on families, and the stability of the health system.

The Senate is expected to reject two partisan measures that would extend Affordable Care Act tax credits enacted during the COVID pandemic, effectively allowing the enhanced subsidies to expire on January first. With both parties failing to engage in substantive high level negotiations, the lapse would mean sharp premium increases for many consumers who purchase coverage on the ACA marketplaces.
Moderate Republicans had advocated for temporary extensions to avert the cliff, but conservative members resisted any change that would alter the law. In the House, Speaker Mike Johnson has promised a vote next week, but without Senate agreement the prospects for averting the expiration are slim. Lawmakers on both sides have signaled the dispute will leave millions of people facing higher out of pocket costs at the start of the year.
Public health experts warn that the loss of subsidies will have immediate and downstream consequences for health outcomes and community health systems. When insurance becomes unaffordable people are more likely to delay preventive care, skip medications, and reduce visits for chronic disease management. Those changes increase the likelihood of emergency department visits and hospitalizations, which in turn strain already stressed health systems and drive up uncompensated care costs.
The communities most at risk are low income households, people of color, and residents of states that did not expand Medicaid. These groups were among the primary beneficiaries of the temporary tax credits, which reduced premiums and out of pocket costs. Without a stable policy response, gains in coverage and in access to preventive services achieved since the pandemic could be reversed, widening long standing disparities in health and financial security.
The political impasse also exposes a structural vulnerability in the American health policy landscape. Relying on temporary measures passed in response to a crisis has left millions dependent on short lived fixes rather than durable changes to affordability. State insurers and marketplaces will need to recalculate premiums and plan offerings quickly, creating uncertainty for consumers and employers during open enrollment season.
Community clinics, rural providers, and safety net hospitals are likely to face increased demand from uninsured and underinsured patients. Local public health programs that extended outreach during the pandemic may be asked to do more with less, while social services and food security programs contend with the ripple effects of sudden cost increases for families.
As the legislative window narrows, advocates are calling for urgent negotiation and for policymakers to consider equitable, long term solutions that address affordability across the income spectrum. Without action, the expiration of the COVID era tax credits will be felt not only in higher premium bills, but in increased barriers to care and deeper strains on communities that have already borne a disproportionate share of the pandemic burden.
Associated Press writers Kevin Freking and Joey Cappelletti contributed to this report.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip