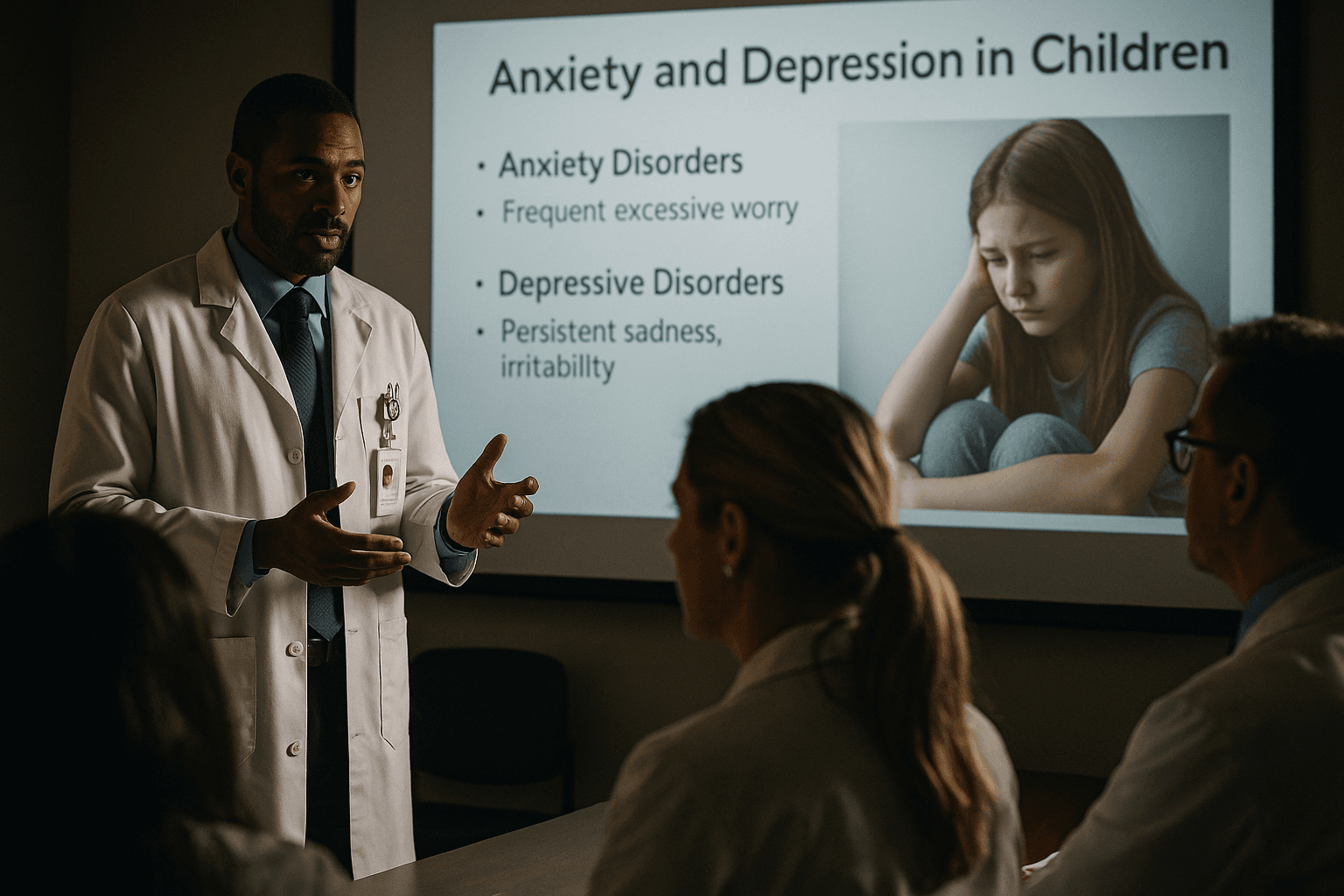
Valley Children’s Trains Primary Care on Pediatric Anxiety and Depression
Valley Children’s Healthcare held a continuing medical education session on December 9 focused on screening and early intervention for anxiety and depression in children, aiming to equip Central Valley pediatric providers with practical tools. The training matters for Fresno County because primary care clinics often serve as the first and sometimes only point of contact for children with mental health needs, and standardized, culturally competent care can help reduce treatment gaps.
On December 9, Valley Children’s Healthcare offered a one hour continuing medical education session for primary care providers titled Mental Health in Pediatric Primary Care: Screening and Intervention for Anxiety and Depression. The presentation, delivered by pediatric psychologist Jessica Louie, PhD, was part of the hospital system’s Quarterly Primary Care Pediatric Provider Educational Series and focused on evidence based screening, early interventions, standardizing patient management, and culturally competent communication.
The session was designed for pediatricians, family medicine clinicians, nurse practitioners, and other frontline providers across the Central Valley who increasingly confront anxiety and depression in young patients. By emphasizing practical, clinic ready approaches, the training sought to make it easier for busy providers to identify symptoms during routine visits, initiate early intervention strategies, and know when to refer to specialty care.
For Fresno County families the program has immediate relevance. Many children here receive most of their health care through community clinics and primary care offices that may lack easy access to pediatric mental health specialists. Standardized screening protocols and communication techniques can shorten the time to diagnosis and treatment, reduce school disruptions, and limit escalation to crisis care. Culturally competent communication is particularly important in the Central Valley where linguistic diversity, varying levels of insurance coverage, and transportation and work schedule constraints can create barriers to care.
Public health implications extend beyond individual clinics. Expanding primary care capacity to manage common mental health conditions can relieve pressure on limited specialty resources, improve outcomes over the long term, and promote equity by delivering care in settings already accessible to underserved populations. Policy considerations include sustainable reimbursement for behavioral health services delivered in primary care and investment in workforce development to expand the number of providers trained in pediatric mental health.
Valley Children’s made registration available through its CME Tracker, at https://www.valleychildrens.org/event/2025/12/09/mental-health-in-pediatric-primary-care-screening-and-intervention-for-anxiety-and-depression. As local demand for pediatric mental health support grows, continued training for primary care teams will be a critical piece of Fresno County’s response.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip