Adjuvant Pembrolizumab Fails to Improve Recurrence‑Free Survival in HCC
At ASCO-GI investigators reported that KEYNOTE-937’s third interim analysis found no recurrence-free survival benefit for adjuvant pembrolizumab versus placebo in hepatocellular carcinoma after curative resection or ablation. The result, coupled with higher immune-related toxicity, reshapes expectations for PD-1 monotherapy in the adjuvant HCC setting and amplifies the need for better patient selection and combination strategies.
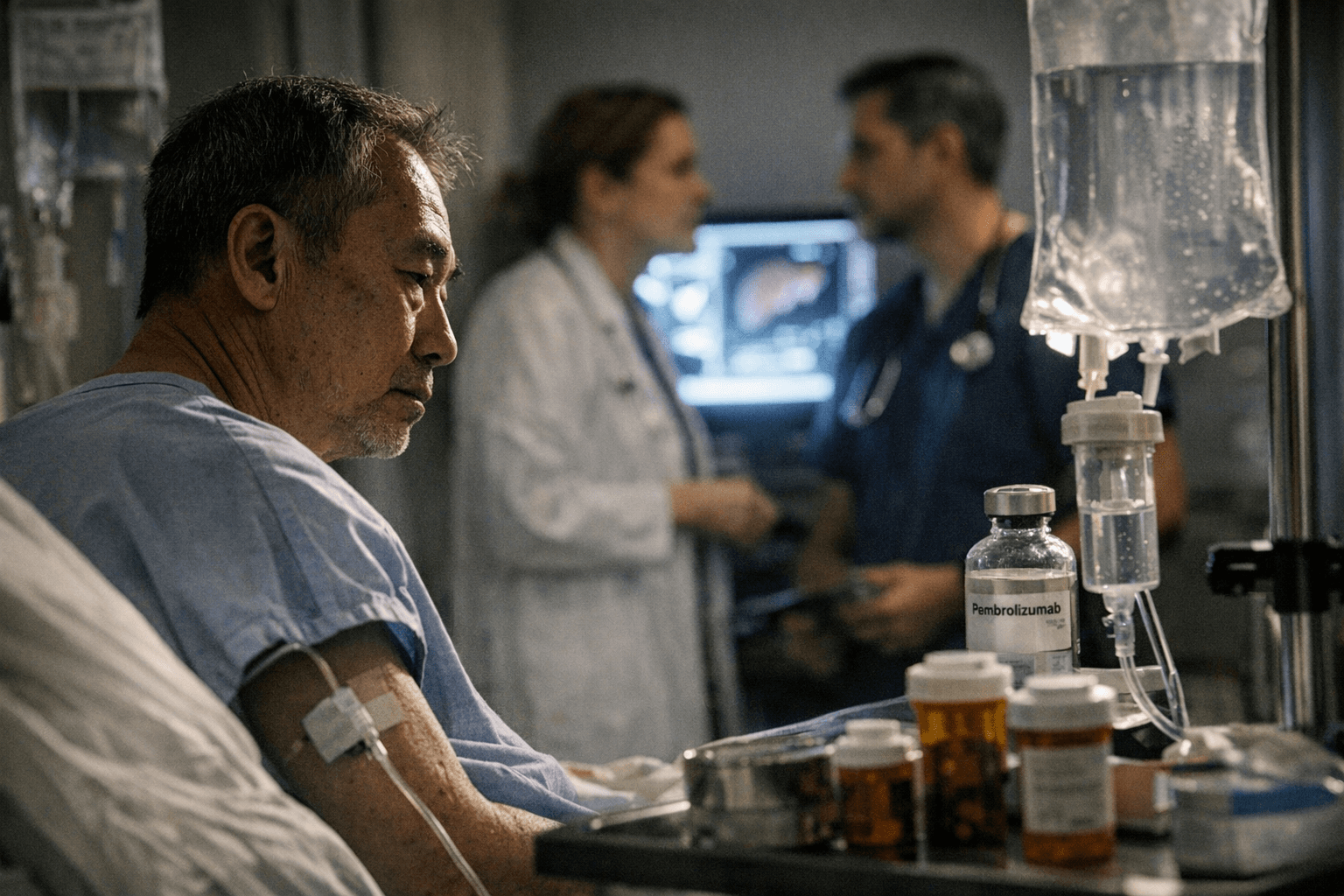
Investigators presenting at the American Society of Clinical Oncology Gastrointestinal Cancers Symposium in San Francisco on Jan. 9, 2026 disclosed that adjuvant pembrolizumab did not reduce recurrence risk in patients with hepatocellular carcinoma who achieved a complete radiologic response after curative-intent resection or local ablation. The third interim analysis of the randomized, double-blind, placebo-controlled phase 3 KEYNOTE-937 trial (NCT03867084) failed to meet its primary endpoint of recurrence-free survival.
Stephen L. (Lam) Chan, MD, FRCP, of the Chinese University of Hong Kong presented the analysis, which used a data cutoff of March 20, 2025 and a median follow-up of 50.7 months. The trial randomized 959 adult patients 1:1 to receive pembrolizumab 200 mg IV every three weeks for up to 17 cycles—stopping earlier for recurrence, unacceptable toxicity, or withdrawal—or placebo. Patients were stratified by region, prior local therapy (resection versus ablation), baseline recurrence risk, and alpha-fetoprotein level at diagnosis. Key eligibility requirements included ECOG performance status 0 to 1 and Child-Pugh class A liver function; patients with recent variceal bleeding, clinically apparent ascites, or hepatic encephalopathy within six months were excluded.
According to the presenters, the primary recurrence-free survival hypothesis was not met at this third interim look. Because the trial’s prespecified hierarchical testing required a positive RFS result before formally assessing overall survival, OS was not tested. The interim report noted no observed benefit in overall survival or in distant metastasis-free survival. Numerical hazard ratios, confidence intervals, and p-values were not disclosed in the summary materials available at the presentation. Safety findings indicated higher rates of treatment-related adverse events in the pembrolizumab arm, including immune-related events, infusion reactions, and an increase in high-grade adverse events, though detailed incidence rates were not provided.
The negative result challenges the premise that PD-1 blockade as a single-agent adjuvant strategy prevents recurrence in early-stage HCC following curative therapy. Recurrence after resection or ablation remains common, and prior to these data no systemic adjuvant therapy had been widely adopted. Recent positive results from IMbrave050, in which atezolizumab plus bevacizumab met a primary RFS endpoint, had raised expectations that immunotherapy-based adjuvant approaches could change practice. KEYNOTE-937’s outcome suggests that PD-1 monotherapy may be insufficient in this setting and highlights the importance of combination regimens or biomarker-driven patient selection.
Clinicians will need complete trial data to evaluate subgroup outcomes, timing and patterns of recurrence, and a granular safety profile before changing practice. The result also underlines ethical considerations in treating patients who may be effectively cured: exposing them to potentially serious immune-related toxicity without clear benefit demands caution. Ongoing phase 3 adjuvant immunotherapy trials, including CheckMate 9DX of nivolumab and other combination studies, will be pivotal to defining effective strategies for preventing HCC recurrence.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip