FDA Approves Itvisma from Novartis for Older Children and Adults with SMA
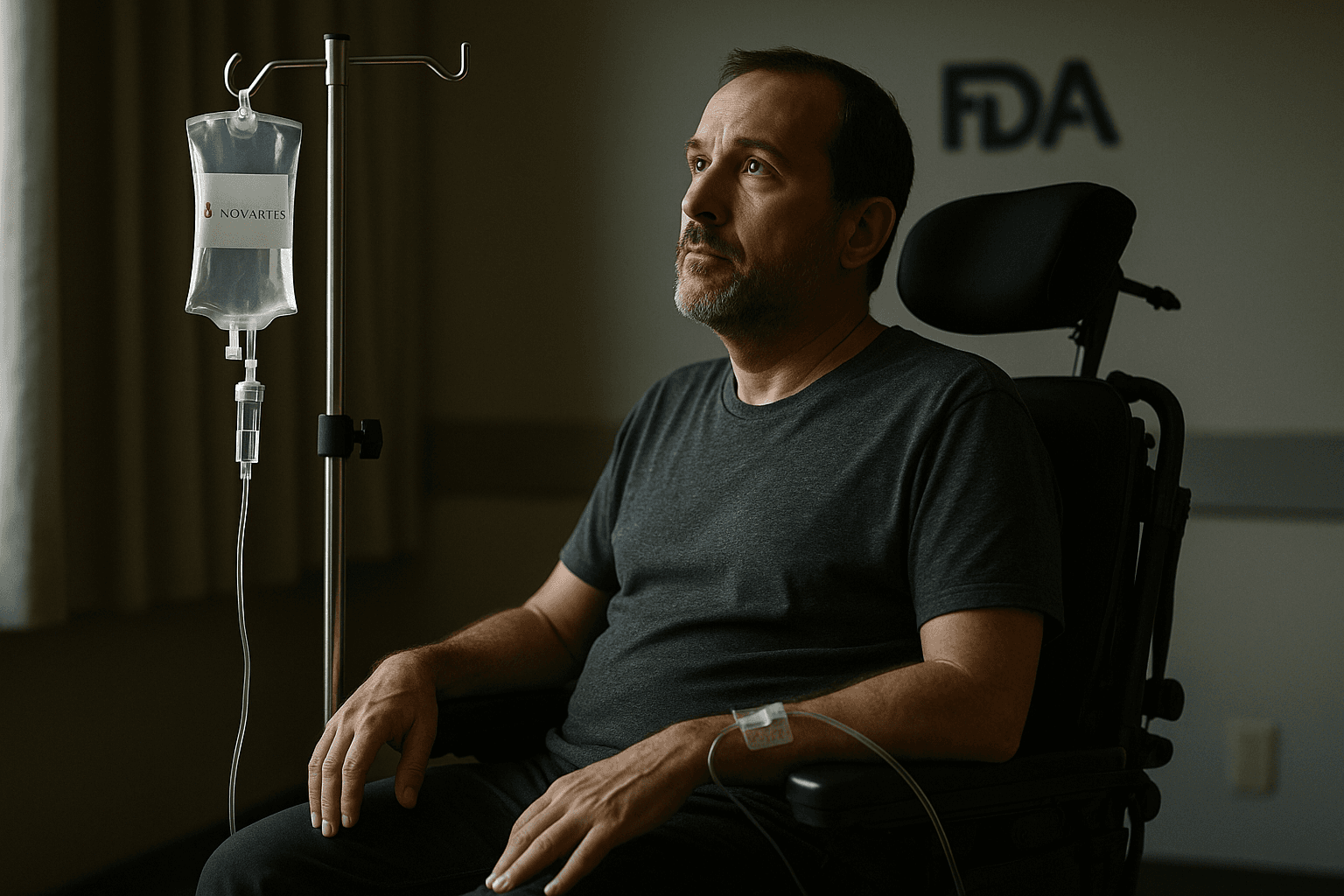
The Food and Drug Administration approved Itvisma, a Novartis gene replacement therapy, for treatment of spinal muscular atrophy in patients aged two years and older. The single dose intrathecal therapy delivers a functional SMN1 gene directly to the central nervous system, expanding options for older children and adults while carrying safety risks that require careful monitoring.

On November 25, 2025, the Food and Drug Administration granted approval to Itvisma, the Novartis gene replacement therapy for spinal muscular atrophy in pediatric and adult patients aged two years and older who have a confirmed SMN1 mutation. The decision follows the agency's priority review and the drug's Breakthrough and Orphan designations, and it was supported by Phase III trial data showing improved motor function.
Itvisma, known generically as onasemnogene abeparvovec brve, is an adeno associated virus vector based therapy given as a single intrathecal infusion to target the central nervous system. The approach delivers a functional copy of the SMN1 gene to motor neurons, addressing the underlying genetic cause of SMA, a progressive neuromuscular disease that leads to loss of muscle strength and mobility. The intrathecal route is aimed at delivering the gene directly into the cerebrospinal fluid, concentrating treatment in the spinal cord and brain.
Regulators noted that Itvisma carries safety risks consistent with earlier SMN1 gene therapies, including hepatotoxicity and other serious adverse events, and the FDA retained boxed warnings where appropriate. Novartis and the agency emphasized that patients receiving the therapy will require careful screening and post treatment monitoring to watch for liver injury and other potential complications. The approval package reflects a balance between demonstrated clinical benefit in motor outcomes and recognized safety concerns that mandate continued surveillance.
The new approval expands one dose gene replacement options to older children and adults, a population that has had limited choices until now. Clinicians and patient advocates have long sought therapies that address disease progression beyond infancy, and regulators said the Phase III evidence was sufficient to recommend use in patients aged two years and above with a confirmed SMN1 mutation. The decision is likely to prompt updates in treatment guidelines and to stimulate discussions among neurologists, geneticists, and payers about appropriate patient selection and timing of administration.
Still unresolved are questions about long term durability, the optimal timing of treatment in older patients, and the management of rare but serious adverse events. Access and affordability will be major issues as health systems and insurers evaluate coverage for a single dose, high cost gene therapy. Manufacturing capacity and the logistics of intrathecal administration at specialized centers will also influence how quickly patients can receive the treatment.
The approval marks a significant step in the evolving landscape of SMA care by offering a gene replacement option for a broader age range of patients. Regulators, clinicians, and advocacy groups will now closely monitor real world outcomes to better understand the long term benefits and risks of this one time genetic intervention.


