Medicaid managed care debate could reshape McDowell health access
State briefings reviewed changes to West Virginia Medicaid, a debate that will affect McDowell County clinics, behavioral health and funding flows.

Representatives of major managed care organizations outlined recommendations to improve efficiencies and reduce costs in West Virginia’s Medicaid program during legislative briefings on January 12. Those proposals framed the hearing, but advocates, providers and rural health leaders pushed back, warning that expanded reliance on managed care could worsen access in remote coalfield communities.
The competing pitches put lawmakers squarely between cost containment and maintaining ground-level services. Managed care groups said tighter networks and administrative reforms would reduce waste and slow program growth. Opponents cautioned that network narrowness, lower reimbursements and heavier administrative burdens can choke off the small clinics and community health centers that serve McDowell County residents, especially for behavioral-health and primary-care needs.
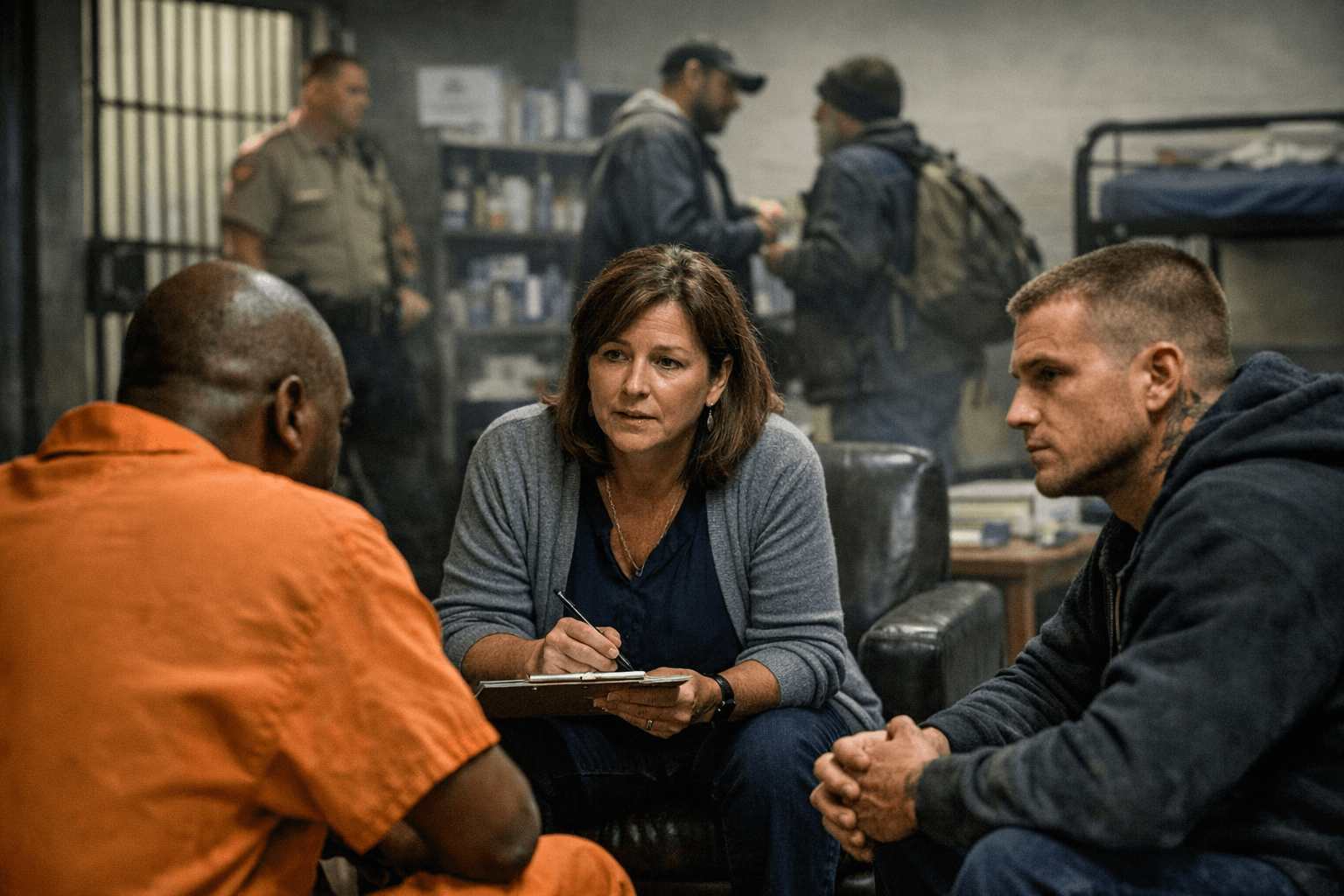
For McDowell County, where clinic closures, workforce shortages and transportation barriers are familiar realities, the policy debate is more than an abstract budget issue. Medicaid payment policies determine funding flows to rural providers that keep doors open in Welch and other hollers. Changes in how managed-care organizations construct networks and authorize services could affect whether a patient can access the same primary care provider, receive timely behavioral-health counseling, or be referred to specialty care without a long drive out of the county.
The briefings also highlighted systemic equity concerns. Rural counties carry higher rates of disability and chronic disease and have fewer providers per capita. Narrower managed-care networks and stricter prior authorization can amplify those disparities unless lawmakers pair cost-savings measures with safeguards for network adequacy, rural provider reimbursement and transportation support.

Lawmakers heard these competing priorities and will now consider next steps as they shape Medicaid policy for the upcoming fiscal cycle. Choices include tightening program controls, adopting targeted investments to shore up rural clinics, or a hybrid path that seeks savings while protecting access in the coalfields. Any change will ripple through hospital budgets, community health centers and behavioral-health services that depend heavily on Medicaid revenue.
Our two cents? Keep an eye on committee meetings and agency rule changes, and bring local stories to your delegates. If policymakers are serious about saving money, they should do it without cutting off care for people who already travel miles for a routine appointment. Practical fixes that protect rural clinics, bolster behavioral-health capacity and ensure network adequacy will matter for McDowell families more than technical accounting tricks.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip