State fines local hospitals including Clovis Community after immediate jeopardy violations
State inspectors fined two Central Valley hospitals in 2025 after finding immediate jeopardy violations tied to a postpartum death, raising local patient safety concerns.

State regulators imposed substantial fines on two Central Valley hospitals during 2025 after inspections found conditions that placed patients in immediate jeopardy, including a $100,000 penalty for Clovis Community Medical Center tied to the avoidable death of a 26-year-old woman.
The fatality occurred after the patient was discharged following childbirth in December 2022; she died of a pulmonary embolism six days later. The state investigation concluded she had multiple risk factors for deep vein thrombosis that were not fully evaluated and that diagnostic testing was not ordered before discharge. Inspectors later returned and found the hospital in compliance after remedial actions were taken.
Clovis Community Medical Center is part of the region’s largest health system. The fines and citations are part of a broader pattern across the Valley in 2025 in which state surveyors issued immediate-jeopardy findings to multiple facilities. The immediate-jeopardy designation signals that a facility’s practices or conditions put patients at significant risk of serious harm or death and requires rapid corrective action.
For Fresno County residents, the case underscores gaps that can occur in postpartum care and hospital accountability. Pulmonary embolism remains a leading cause of maternal death nationwide, and early recognition of deep vein thrombosis risk is a key preventive step. When assessment, testing, or follow-up planning fail, the consequences can be devastating for young families and for communities already facing barriers to care.
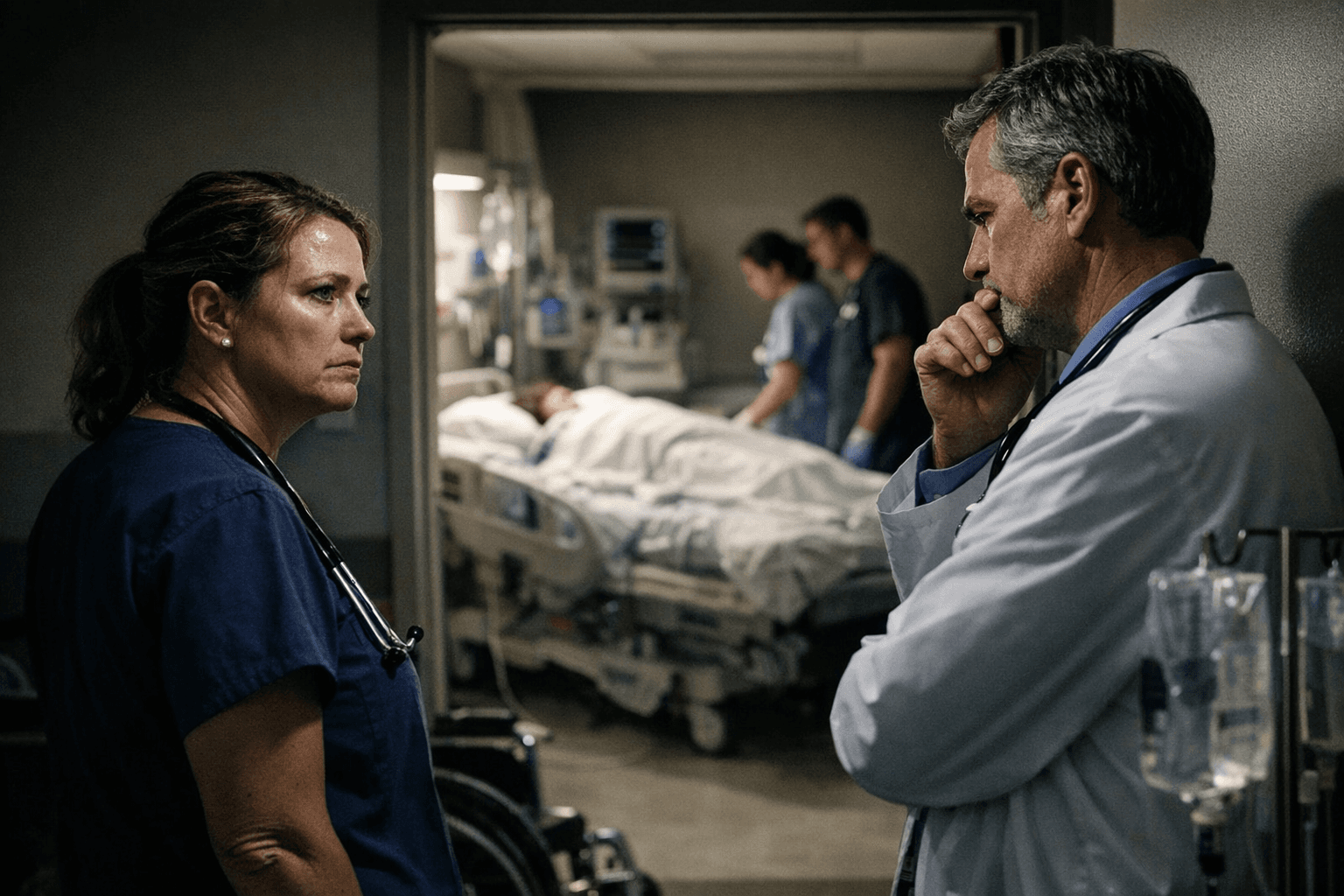
Hospital leaders in the cases cited have said they implemented policy changes and corrective steps after the inspections. Regulators’ return visits that found compliance illustrate the role of oversight in forcing rapid improvements, but they also highlight the reactive nature of enforcement — changes often come after a serious event.
Public health implications extend beyond any single hospital. In communities across the Central Valley, factors such as language barriers, transportation challenges, limited access to primary care, and workforce shortages can complicate postpartum follow-up and risk monitoring. When hospital systems miss opportunities to evaluate risk or order diagnostic testing, those systemic pressures are part of the context that can turn a routine discharge into a life-threatening situation.
The takeaway? Ask direct questions before discharge about your risk for blood clots, what symptoms to watch for, and what the follow-up plan will be. Keep postpartum appointments, seek care immediately for leg pain or sudden shortness of breath, and if you have concerns about a hospital’s response, notify public health authorities or your clinician. Our two cents? Trust your instincts and press for clear discharge instructions — it could make all the difference for you or someone you love.
Sources:
Know something we missed? Have a correction or additional information?
Submit a Tip

