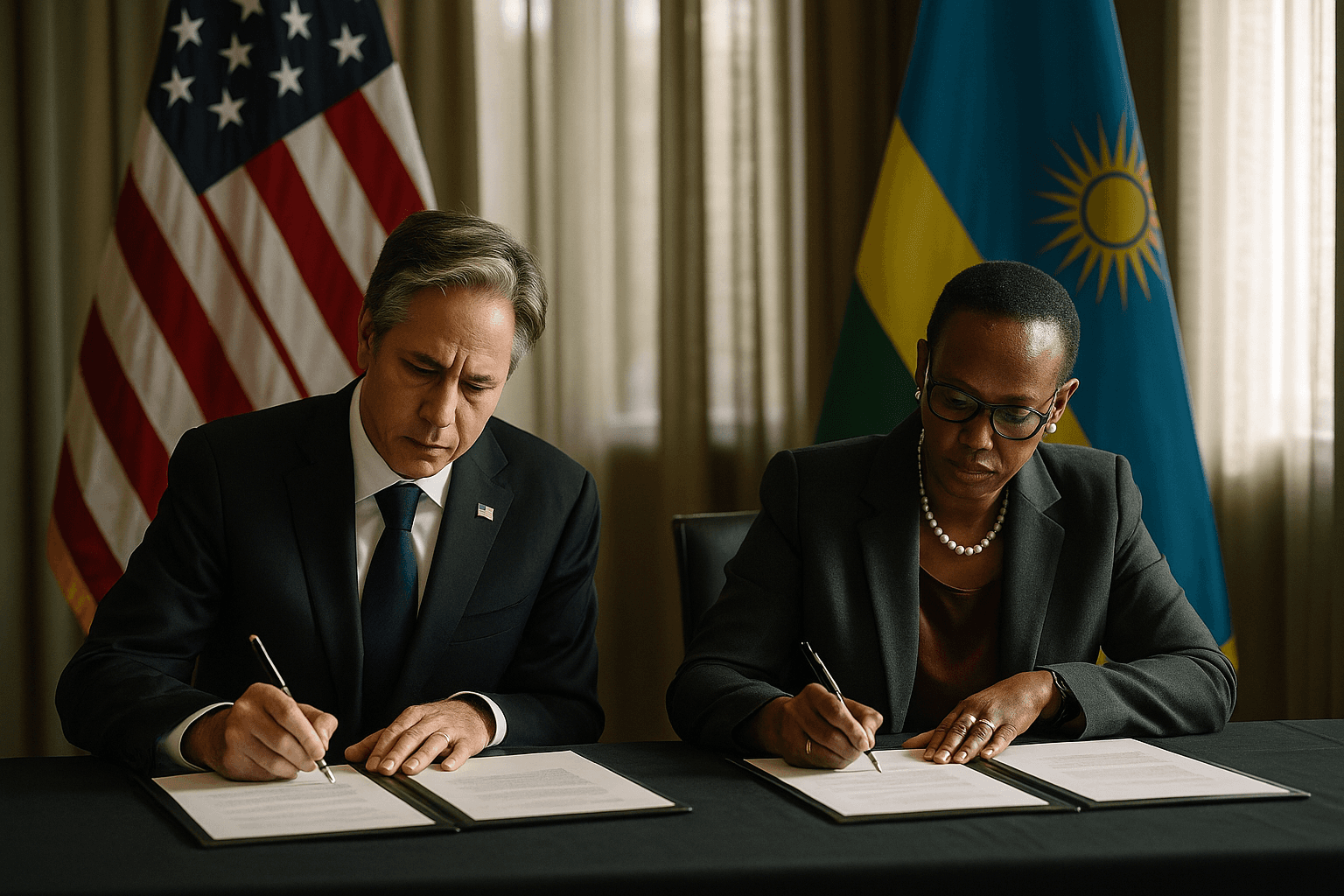
United States and Rwanda sign $228 million health pact, shift aid model
The United States and Rwanda signed a five year agreement committing $228 million to strengthen Rwanda's health sector under the administration's America First Global Health Strategy. The pact pairs up to $158 million in U.S. funding for HIV, malaria and infectious disease work with a Rwandan pledge to increase domestic health spending by $70 million, raising questions about sustainability, equity and local accountability.

In Kigali on December 6, the United States and Rwanda sealed a five year agreement that will direct $228 million toward strengthening Rwanda's health system under the administration's America First Global Health Strategy. The arrangement commits up to $158 million from the United States to support HIV AIDS, malaria and infectious disease programs while boosting disease surveillance and outbreak response. Rwanda agreed to increase its own health spending by $70 million over the life of the deal.
Rwandan officials framed the package as an opportunity to expand services and reinforce public health infrastructure. For public health planners, the funds promise targeted investments in laboratory networks, rapid response capacity and continued HIV treatment and prevention programs that have been central to Rwanda's progress over the past two decades. The agreement is the second of its kind under the administration's new aid approach which emphasizes country self reliance and co financing.
The model represents a deliberate shift from traditional aid relationships that prioritize direct donor funding for specific initiatives. By requiring greater domestic financial commitment, co financing is intended to promote national ownership and long term sustainability of health programs. In practice, the approach will test whether modest increases in domestic spending can be matched to international technical assistance to sustain gains against HIV AIDS and malaria while improving readiness for future outbreaks.
Public health implications will depend on how the money is allocated and how quickly Rwanda can translate the pledged $70 million into strengthened frontline services. Incremental domestic funding may improve health worker salaries, clinic supplies and community outreach if directed toward primary care and prevention. It may also accelerate investments in digital surveillance systems that can detect and contain outbreaks early, a priority for global health security.
At the same time, the co financing framework raises equity concerns. Requiring recipient countries to shoulder a larger share of program costs can squeeze already constrained budgets, forcing difficult trade offs between health priorities and other social services. The impact is felt most acutely by vulnerable communities who rely on publicly funded clinics, including women, children and people living in rural areas. Advocates caution that without robust safeguards for equity, gains against infectious disease could be uneven and fragile.
Accountability and transparency will be central to assessing the pact's success. Clear benchmarks for service coverage, measurable improvements in surveillance, and independent monitoring of expenditures will be necessary to ensure that funds reach patients and communities rather than being absorbed by higher level administrative costs. The United States funding is described as up to $158 million, signaling that disbursement may be conditional on performance or other criteria.
As donor strategies evolve, the agreement with Rwanda offers a real world test of whether co financing and greater national responsibility can coexist with commitments to equity and universal access. For communities on the front lines of disease burden, the outcome will be judged not by policy statements but by whether clinics stay open, medicines remain available and surveillance systems prevent the next outbreak from becoming a crisis.


