U.S. and Rwanda sign $228 million health pact, shifting costs to Rwandan budget
The United States and Rwanda signed a five year, $228 million health agreement that will channel U.S. funding into infectious disease control while asking Rwanda to increase domestic health spending by $70 million. The deal is part of the Trump administration's "America First Global Health Strategy" and raises questions about sustainability, equity, and regional health security.

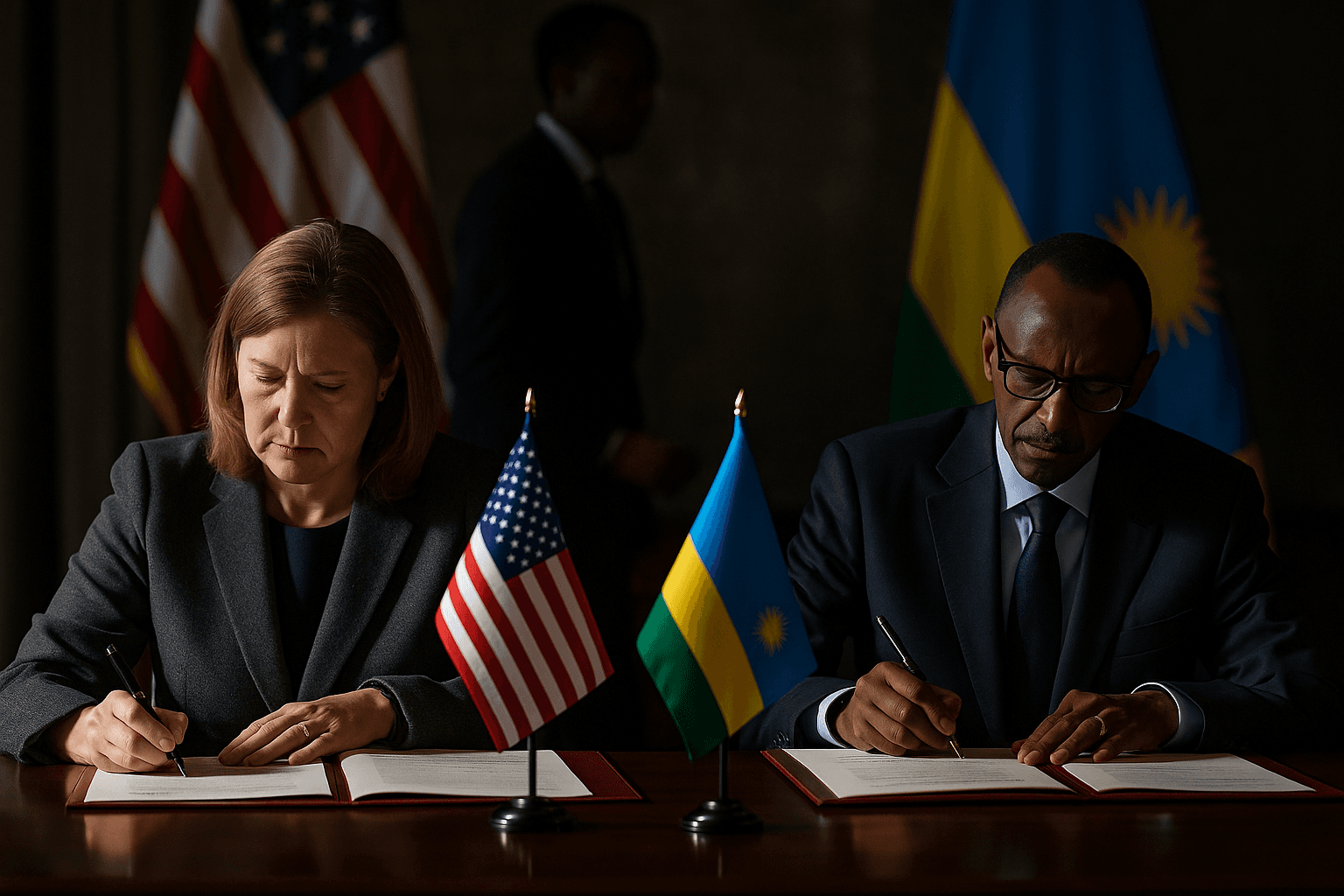
The United States and Rwanda formalized a five year, $228 million partnership on December 6 that aims to bolster Rwanda's capacity to prevent and respond to infectious disease while accelerating a transfer of financial responsibility to Kigali. The State Department said the pact is the second under the Trump administration's "America First Global Health Strategy" and commits up to $158 million in U.S. support to fight HIV AIDS, malaria and other infectious diseases, strengthen disease surveillance and outbreak response, and fund broader health sector improvements.
Under the terms of the agreement Rwanda has agreed to expand its own health investment by $70 million during the period, effectively sharing the cost of programs that previously relied more heavily on donor financing. The move follows a larger, $2.5 billion U.S. partnership with Kenya announced this week, reflecting a broader shift by Washington toward bilateral, host country agreements rather than channeling funds through multilateral mechanisms.
Public health experts say stronger surveillance and outbreak response systems are vital to detecting and containing threats early, a capacity that benefits both Rwanda and its neighbors. Building on delivery innovations such as Zipline's drone distribution of medical supplies, the pact seeks to modernize logistics and reduce delays in delivering essential drugs and diagnostics to remote clinics. Those advances are likely to make care more reliable in rural communities that have historically faced access barriers.
The emphasis on domestic financing and bilateral negotiation carries potential benefits, including greater alignment of aid with national priorities and increased ownership of programs. Yet the rebalancing also introduces risks for equity and continuity of care. Shifting costs onto national budgets can strain health services in lower income settings where fiscal space is limited, threatening progress against chronic conditions and undermining support for vulnerable groups including the rural poor, people living with HIV, and women who rely on primary care services.
For frontline communities the impact will depend on how Rwanda allocates the additional $70 million in domestic health spending. If funds are directed toward community health workers, primary clinics and supply chains, they could sustain and deepen recent gains in maternal and child health and infectious disease control. If fiscal pressures lead to prioritization of high visibility projects at the expense of day to day care, disparities may widen.
The pact comes amid broader diplomatic activity in the Great Lakes region, including talks tied to an international effort to stabilize eastern Congo. Stronger surveillance and cross border cooperation could reduce the risk of outbreaks spreading across porous frontiers, a public health imperative in a region that has faced repeated outbreaks of Ebola and cholera.
The five year timetable will provide a framework to assess outcomes, but transparency and measurable milestones will be crucial to determine whether the new approach yields sustained improvements in health outcomes and equity. As donor patterns change, advocates and policymakers will be watching whether technology driven delivery innovations are matched by investments in workforce, community based services and the persistent, less visible components of health systems that most affect everyday access to care.


